Designing Medical Devices for People with Autoimmune Diseases: Embracing Flexibility and Empathy
Jul 10, 2025
This article was written by Amanda Bakkum, Human Factors Consultant at ClariMed.
When designing medical devices for people with autoimmune diseases, one of the most critical yet often overlooked challenges is the day-to-day unpredictability of symptoms. Unlike many conditions that follow a more stable course, autoimmune diseases—such as lupus, rheumatoid arthritis, and multiple sclerosis—can bring sudden waves of fatigue, joint pain, brain fog, and muscle weakness with little warning. To make matters worse, people living with these conditions often don’t look sick, even when they are experiencing significant pain, fatigue, or other debilitating symptoms. This can lead to misunderstandings, lack of support, and judgment from others—making daily life more challenging both emotionally and physically.
The day-to-day variability and invisibility of symptoms demand a different design mindset: one rooted in adaptability and empathy.
A useful framework to understand this lived experience is “The Spoon Theory”, a metaphor developed by Christine Miserandino [1]. It suggests that people with chronic illness start each day with a limited number of "spoons," or units of energy. Basic tasks like getting dressed or making breakfast each consume a spoon, leaving fewer available for other needs. On difficult days, even the smallest task can feel like a monumental effort, forcing users to carefully prioritize how they allocate their spoons.
Designing for "spoonies" means creating devices that are not only easy to use when someone is feeling well, but also forgiving and supportive when they are not. At the core, inclusive medical design for autoimmune users isn't just about functionality—it's about honouring resilience and recognizing the reality of living with an unpredictable body. The goal is to empower patients, one thoughtful feature at a time.
How Human Factors Engineering Helps
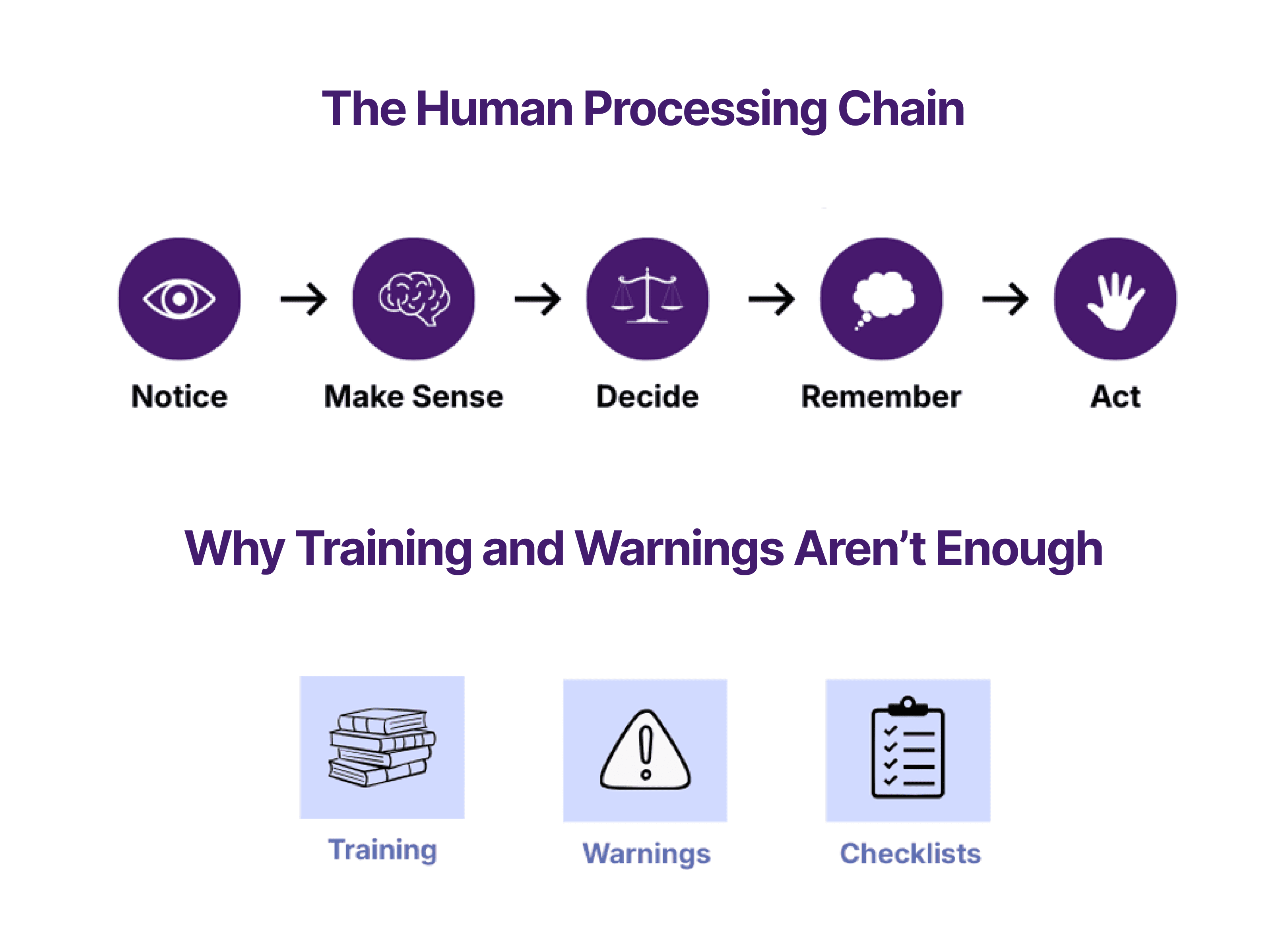
Human Factors Engineering (HFE) focuses on designing systems and products that align with how people actually interact with them, especially under stress, fatigue, or other limitations. It plays a pivotal role in ensuring medical devices are not only functional, but truly usable by people with fluctuating physical and cognitive abilities.
Here’s how HFE translates into better, more inclusive medical devices for people with autoimmune conditions:
1. Designing for Day-to-Day Variability
HFE research involves deeply understanding user needs in different states, not just on their best days. This means accounting for pain, stiffness, mental fog, and limited mobility.
Design implication: Devices must be as easy to use on a flare-up day as on a good one, ensuring consideration is given to the physical constraints specific to individual conditions.
2. Ergonomics for Limited Strength and Dexterity
Autoimmune diseases often affect fine motor skills. Devices must work well even when hands are weak, joints are swollen, or tremors occur.
HFE response: Large, soft-touch buttons, minimal force requirements, and shapes that don’t require tight grips or awkward hand positions.
3. Minimizing Cognitive Load
Brain fog can make even simple tasks overwhelming. Interfaces should reduce the mental effort required to operate a device.
Design tactics: Use of clear icons, step-by-step guidance, gentle voice prompts, and minimal screen clutter.
4. Supporting Error Prevention and Recovery
Mistakes happen—especially when users are fatigued. Devices should guide users gently and provide simple ways to recover from errors.
HFE principle: Fail-safe design, undo functions, and friendly error messages can make a huge difference.
5. Emotional Design: Building Trust and Confidence
Using a medical device shouldn’t feel like a chore or a test of endurance. Devices should feel supportive, intuitive, and even empowering.
Why it matters: A device that feels like an ally—not a burden—builds trust, promotes adherence, and supports mental well-being.
6. Building with Empathy
Designing for people with autoimmune diseases means recognizing that every day is different. It means asking questions like:
What if the user can’t grip anything today?
What if they’re too mentally foggy to follow complex steps?
What if they only have two “spoons” left when it’s time to use this device?
The answers to these questions aren’t obstacles—they’re design opportunities. Human factors engineering gives us the tools to respond with intelligence and compassion.
Bottom Line
When we design with variability, empathy, and human reality in mind, we do more than create accessible medical devices—we restore independence and dignity for people managing chronic illness. That’s the true power of thoughtful design.
References
[1] Miserandino, C (2003). The Spoon Theory. https://www.butyoudontlooksick.com/articles/written-by-christine/the-spoon-theory/